Donna Simmons
Board Chair

Donna Thompson
CEO
Looking Forward
Over the last year, the health care industry has continued to experience a great deal of volatility and change. Some developments have negatively impacted our vulnerable patient population while other changes have brought new opportunities to improve our standards of care and explore new avenues to impact the health of our communities.
In the face of this ever changing landscape, ACCESS has remained committed to its mission and vision, and continues to work on the key strategic initiatives set forth in our FY’17-FY’19 Strategic Plan, which is included in this report. It has not always been an easy journey for us but by being nimble and disciplined in our approach to care and innovation, we have been able to continue to find new and better ways to serve the more than 181,000 patients who depend on ACCESS as their medical home each day.
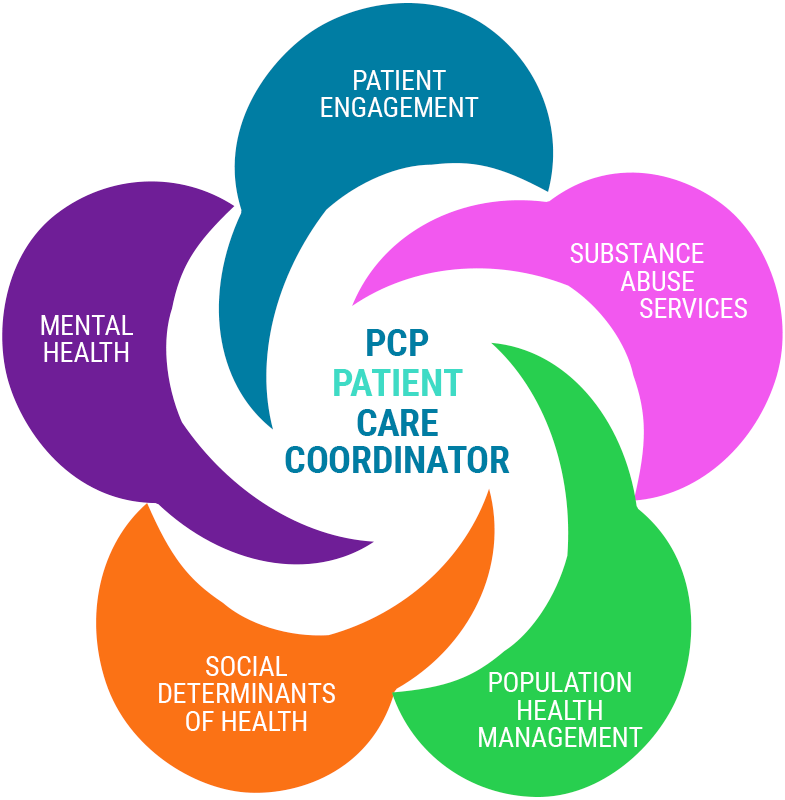
Much of our work over the past year has been focused in one critical area: shifting from a fee-for-service model to a value-based care model. While this is a huge paradigm shift for health care providers, it has given us an opportunity to better engage our patients in a planned approach to care. We have invested in building our care coordination expertise to meet patients where they are at all points of care. In this report, you will find out how we have expanded our care coordination services to embed care coordinators right in the emergency rooms of key hospital partners. From equipping nurses in the E.R. with an ACCESS patient’s vital medical history to giving our managed care partners direct access to schedule appointments for members on Day One, we continue to leverage our investment in Epic, our electronic health record, to impact patient access to care and ultimately, better quality outcomes.
Through our strategic plan and mission, we have also re-examined our community partnerships to find the right organizations that are aligned with our goals to improve those health outcomes. In this report, you will learn about two new, innovative collaborations. One pilot embeds a Legal Council for Health Justice lawyer right in one of our health centers to assist with legal issues that may be affecting a patient’s health. Another pilot extends our food for health partnership with the Greater Chicago Food Depository in a whole new way through a meal delivery program for high-risk patients. At the end of day, we know that the Chicagoland area is full of amazing organizations doing great work in our communities. Our challenge going forward is to leverage the strengths of those organizations, our combined resources and collaborate in more meaningful ways to impact real change in our communities.
We know the road ahead will continue to bring new challenges and opportunities for improvement and innovation. As one of Chicago’s leading health care providers to the underserved, our charge will always be to make the right decisions for our patients. We hope you enjoy this report’s glimpse into our ongoing journey to deliver the best care possible and transform the health of our communities.
In Good Health,
Donna Thompson
CEO
Donna Simmons
Board Chair
I know that there are a lot of people like me who feel as if they don't have anyone to turn to or anywhere to go. I want to let people know that they can get through this. Without ACCESS, I would never have done the footwork needed to complete school,” said ACCESS Westside Family Health Center patient Angela Scott, who now has dreams of paying it forward and becoming a certified drug and alcohol counselor herself.
| 2017 | 2016 | |
|---|---|---|
Assets |
||
| Cash & Cash Equivalents | 5,677,261 | 20,551,719 |
| Patient Accounts Receivable, Net | 8,017,777 | 5,166,789 |
| Managed Care Receivables | 1,822,199 | 1,757,809 |
| Contracts and Grants Receivables | 1,496,906 | 2,244,897 |
| Other Receivables | 3,892,778 | 2,109,870 |
| Investments | 1,331,963 | — |
| Prepaid Expenses & Other Assets | 1,549,726 | 1,737,151 |
| Total Current Assets | 23,788,610 | 33,568,235 |
| Total Property & Equipment | 25,560,175 | 27,269,082 |
| 457(b) Plan Participant Assets | 1,628,829 | 1,334,157 |
| Other Assets | 765,995 | 731,395 |
| Total Assets | 51,743,609 | 62,902,869 |
Liabilities and Net Assets |
||
| Current Liabilities | 14,410,792 | 30,508,051 |
| Long-term Liabilities | 6,418,699 | 6,473,186 |
| Total Liabilities | 20,829,491 | 36,981,237 |
| Net Assets | ||
| Unrestricted | 29,051,260 | 3,778,538 |
| Temporarily Restricted | 1,862,858 | 2,143,094 |
| Total Net Assets | 30,914,118 | 25,921,632 |
| Total Liabilities and Net Assets | 51,743,609 | 62,902,869 |
| 2017 | 2016 | |
|---|---|---|
Revenue And Other Support |
||
| Patient Service Revenue | 59,716,068 | 61,175,057 |
| Managed Care Revenue | 20,970,065 | 23,364,598 |
| 340B Pharmacy Revenue | 22,252,608 | 19,317,421 |
| Contributions & Grants | 21,827,182 | 23,101,127 |
| Gain on Settlement of Third-Party Liability | 6,849,190 | — |
| Other Revenue | 2,669,242 | 2,531,618 |
| Total Revenue and Other Support | 134,284,355 | 129,489,821 |
Operating Expenses By Function |
||
| Program Services | 100,125,968 | 94,441,139 |
| Management and General | 29,165,901 | 27,565,779 |
| Total Operating Expenses | 129,291,869 | 122,006,918 |
| Change in Net Assets* | 4,992,486 | 7,482,903 |
Hover over charts for more detail.
Revenue
Contributions & Grants
Encountor Payor Mix
Operating Expenses
Education opens doors to success. I am honored, and I thank ACCESS for giving me this opportunity to be able to pursue my educational goals.”
A total of 0 Employees Awarded Educational Scholarships • $ 0 awarded to date
ACCESS Board of Directors
To assure quality and responsiveness to community health needs, more than half of Access Community Health Network’s Board of Directors are patients. The asterisk (*) identifies patient representatives.
- Chair Emeritus
- Bena Sullivan*
- Chair
- Donna Simmons*
- Vice Chair
- Thomas P. FitzGibbon, Jr.*
- Treasurer
- Terry Brown
- Secretary
- Perla Herrera*
- Members
- Patti Bobb
- Charles DeShazer, M.D.
- Sharon Gibson*
- Lilia Gonzalez*
- Ryan Hart*
- Denise Kitchen
- Daniella Levitt
- Miriam Mobley-Smith
- Pete McNerney
- Erick Osorio*
- Virginia Oviedo
- Eve Salazar*
- Erin Starkey, L.C.S.W.*
- Liz Vazquez*
ACCESS Senior Leadership Team
- Donna Thompson, R.N., M.S.
- Chief Executive Officer
- Jairo Mejia, M.D.
- Chief Medical Officer
- Ann Lundy, R.N., B.S.N., M.B.A.
- Chief Operating Officer
- Mahomed Ouedraogo, B.S., C.P.A.
- Chief Financial Officer and Interim Chief Information Officer
- Etta Ish Henderson, B.A., M.P.H.
- Chief Compliance Officer
- Eleva Riley, M.A.
- Vice President of Human Resources
- Cristina Sotelino
- Vice President of Communications and Community Engagement
- Tariq Butt, M.D.
- Vice President of Health Affairs
FY’17 Private Grantors
ACCESS extends its appreciation to the many donors who partner to provide health care services for the underserved members of our community. Every gift plays an integral role in the success of our organization’s mission. ACCESS thanks the following corporations, foundations and organizations for their support in FY’17 (July 1, 2016 – June 30, 2017).
FY ’17-‘19
ACCESS Community
Health Network
Strategic Plan
Patient Engagement
ACCESS is the health care home of choice and is committed to creating an experience at all points of care in partnership with patients to manage their total health.
Strategic Partnerships
ACCESS has an integrated network of partners with high quality services and data to address the medical, behavioral, social and economic factors that have the greatest impact on health outcomes and total cost of care.
Financial Future
ACCESS has a strong business model, which leverages its financial strength and assets to invest in workforce, technology, integrated systems and infrastructure to support growth and transform care.
Workforce Engagement
ACCESS has a culture that develops, recognizes and rewards our diverse workforce in an environment that promotes teamwork, communication and transparency.
Leadership In Community Health
ACCESS is an advocate for health equity, partnering to develop best practices in community health and share solutions to improve population health outcomes.